State-of-the art drug screens for neurodegenerative diseases
What if a drug already being safely used by the population could also help treat a different, unrelated disease? With 1000s of drugs available, and more being developed in labs across the globe, drug screening is vital to make sure potential treatments for diseases are not being missed.

Drug screening is a process that allows scientists to test drugs or drug-like compounds to see if they have any beneficial impact on health conditions. Scientists at the 91Ö±²„ Institute for Translational Neuroscience (SITraN) are drug screening for potential new treatments for neurodegenerative diseases.
The process of drug screening sounds like something straight out of a sci-fi novel. Skin cells are taken from patients and grown in culture or reprogrammed into either neurons or glia - the support cells of the nervous system. The patient derived cell cultures are then used to test libraries of drug compounds, in the hope of identifying new treatments for various health conditions including Alzheimerās disease, Parkinsonās disease and motor neuron disease (MND).
The screening process at our state-of-the-art Drug Discovery lab is twofold. Drug compounds are tested to see they have a beneficial impact on any neurodegenerative diseases. Once a compound has been identified as beneficial, researchers may need to develop it further to ensure it is optimised for medical use.
Repurposed drug screens, however, identify drugs already in medical use that can be repurposed to treat neurodegenerative diseases. If the beneficial compound is already certified as safe, it can move straight to clinical evaluation for a new purpose in patients. Screening drugs that are already approved for other uses can save years and hundreds of millions of pounds.
Specialist facilities
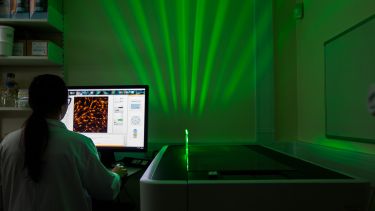
Inside the Drug Discovery lab at SITraN, you will find a range of specialist equipment usually found in pharmaceutical environments, not academic settings. It contains libraries of drugs and drug-like compounds optimally stored to test on patient models. These facilities, alongside the expertise of our scientists, allow us to run extensive drug screening programmes.
Over the last 10 years, we have had notable success working with pharmaceutical companies to identify new treatments for neurodegenerative disorders.
Our ambition is to expand our drug screening capability with a specialist building dedicated to working with pharmaceutical organisations to make more treatments available to patients at a faster rate.
Potential new treatment for motor neuron disease (MND) identified
Through drug screening, researchers at SITraN identified neuroprotective properties in a drug candidate known as M102. Preclinical models showed the potential for M102 to significantly slow or reverse MND progression, which affects a patientās ability to walk, talk, eat and breathe, in both familial and sporadic MND patients.
The drug candidate activates the NRF2 (nuclear factor erythroid 2-related factor 2) and HSF1 (Heat shock factor 1) signalling pathways, recently understood as important disease pathways in MND.
A recent grant, awarded by Australian charity FightMND, will support SITraNās partnership with Aclipse Therapeutics to progress M102 into first in-human trials for patients with the neurodegenerative disease.
This therapy may also be of benefit in other neurodegenerative conditions including, Friedreichās ataxia, Huntington's disease and Parkinson's disease.
M102 has properties which allow multiple protective pathways to be activated within the nervous system. We are very hopeful that it may have beneficial effects in slowing the progression of MND.
We are very excited for MND patients, as FightMND is supporting our effort to advance this important therapy - which was discovered in SITraN as a neuroprotective molecule and which looks so promising in preclinical models - into clinical trials for our patients.
Professor Dame Pamela Shaw
Director of SITraN, the Neuroscience Institute and the NIHR 91Ö±²„ Biomedical Research Centre
Can a drug used to treat liver disease also help treat Parkinsonās and Alzheimerās disease?
Researchers at SITraN are taking part in two pioneering studies to investigate a liver drug, ursodeoxycholic acid (UDCA), and its effects on mitochondria - or the cellās batteries.
Mitochondrial dysfunction is a significant factor in both Parkinsonās and Alzheimerās disease. Therefore, a drug that could boost mitochondrial performance has the potential to slow the progression of these diseases.
Researchers identified UDCA as the most promising drug to rescue mitochondrial function in a drug screen where 2,000 drugs were assessed for their rescue effect in Parkinsonās disease.
Now, SITraN researchers, in partnership with 91Ö±²„ Teaching Hospitals NHS Foundation Trust, will assess the safety and tolerability of UDCA in Parkinsonās patients. It is hoped that eventually UDCA can be repositioned to slow down and even reverse the progression of Parkinsonās disease.
After nearly a decade of research, we are extremely pleased to launch the first clinical trial of UDCA in Parkinsonās patients to see if the drug is safe and tolerated. This is a pilot trial, which if successful, will lead to a bigger study to firmly establish the effectiveness of the treatment to slow down progression of Parkinsonās.
Professor Oliver Bandmann
Professor of Movement Disorders Neurology, NIHR BRC 91Ö±²„ Investigator and Honorary Consultant Neurologist at 91Ö±²„ Teaching Hospitals NHS Foundation Trust
Similarly, a study funded by Alzheimerās Research UK, is taking place to investigate if UDCA is beneficial to people living with Alzheimerās disease.
As the drug is already in clinical use for liver disease, this speeds up the potential time it could take to get this drug to the clinic for patients. Most importantly, we found the drug to be active in cells from people with the most common type of the devastating disease ā sporadic Alzheimerās ā which could mean it has potential for thousands of patients.
Dr Heather Mortiboys
Senior Lecturer in Translational Neuroscience and Parkinson's UK Senior Research Fellow
Artificial Intelligence looks for candidate drugs
British artificial intelligence company BenevolentAI is using machine learning to have computers do the reading for us. They are conducting unbiased literature searches and scouring chemical databases to suggest compounds that could have a therapeutic effect in diseases like MND.
SITraN researchers, Dr Richard Mead and Dr Laura Ferraiuolo tested one such candidate emerging from BenevolentAI in patient cell models and found that it delayed the onset of the disease and prevented death of motor neurons.
This is an exciting development in our research for a treatment for MND. BenevolentAI came to us with some newly identified compounds discovered by their technology. Two of which were new to us in the field and, following this research, are now looking very promising. Our plan now is to conduct further detailed testing and continue to progress promising findings toward new treatments.
Dr Richard Mead
Senior Lecturer in Translational Neuroscience
Developing a drug screen for C9ORF72 gene mutations
A single gene mutation can cause either motor neuron disease (MND) or fronto-temporal dementia (FTD), and sometimes both. This tells us that the mechanisms of these diseases are related and only differ by the nerve cells that are affected. Thatās because these diseases are complicated and neurodegeneration arises as a result of the interplay between genetics and the environment.
The resulting biological products from this mutation is aberrant RNA and protein. This causes a burden and toxicity to the cell that emerges with age.
In SITraN, we have helped with the global understanding of this gene function, showing it has a role in autophagy - the cell's waste disposal route for removing damaged proteins - which may help with future therapies.
Researchers are developing models so that they can screen for both removal of the pathological burden, whilst improving the function of the biological pathway identified. This will allow them to identify how the compounds are working so they can better predict any possible side effects, or better still, avoid side effects completely.
To find out more about our drug screenings please contact Sara Lancashire on s.j.lancashire@sheffield.ac.uk